A 60 year old female presented to us with altered sensoriom and headache vomitings. MRI BRAIN revealed large posterior fossa mass with hydrocephalus. Patient underwent Left sided VPMP shunt followed by complete tumour removal with good outcome.
Mri showing large posterior fossa mass.
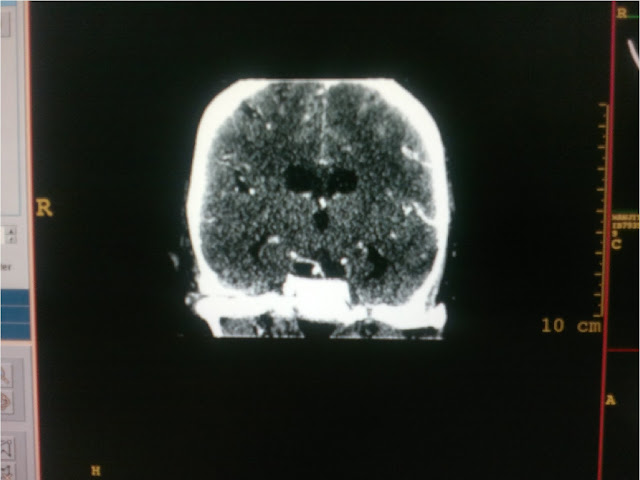
CT showing complete tumour removal.
Neurosurgeon in India
Saturday, 13 February 2016
Large posterior fossa mass operated by Dr Vineet Saggar consultant neurosurgeon mohali
Thursday, 12 June 2014
ADVANCED SPINE SURGERY : IMAGES
CASE OF JUMPED FACETS FOLLOWING CERVICAL SPINE INJURY

A CASE OF MULTIPLE VERTEBRAL FRACTURES FOLLOWING FALL FROM HEIGHT

X RAYS FOLLOWING FIXATION AT TWO LEVELS PATIENT JUST BEFORE DISCHARGE
PEDICLE SCREW FIXATION FOR LISTHESIS L5 -S1
Monday, 25 November 2013
FOOT BALL MENINGIOMA OPERATED AT IVY HOSPITAL BY DR VINEET SAGGAR
Meningiomas account for 15% of intracranial tumors and 90 percent of meningiomas are intracranial. They commonly occur in the fourth through sixth decades of life. They are more common in females and are rare in children. Meningiomas are brain tumors which do not arise from the cells of the brain (as against glioms which arise from glial cells and other tumors which arise from neural cells). As they do not arise from “brain” cells, they actually are extra-axial in location. By that I mean, they are located outside the brain but inside the skull. So meningiomas do not actually “invade” the brain, on the other hand as they grow in size they press on the brain from outside inwards. Meningiomas are slow growing tumors and as I stated earlier they usually do not invade the brain (though they may be locally invasive at times and these tumors are called atypical or malignant meningiomas).
Since these tumours are slow growing they can achieve enormous sizes before causing symptoms . there are areas in brain which are non eloquent ( areas which are non vital to daily functioning of brain ) such as frontal sub frontal areas , these tumours can achive huge sizes before causing any deficits . Such tumours are akin to large FOOTBALLS in brain . Removal of these tumours require patience and and long duration surgeries and some times tumour is removed sub totally in first attempt and to avoid complications of prolonged surgery in one go rest of tumour is removed next 1-2 days
SIGNS AND SYMPTOMS OF MENINGIOMAS DEPEND UPON THEIR LOCATION
Vision Changes
Meningioma that grows on the bгain mаy cauѕe vision problems, such аs blυrred οr double vision or vision loss.
Hearing Lοss
Hearing loss is а sүmptom οf meningioma near tһe аuditory nerνes oг the bones of the eаr
Headaches
Aсcording to the Mаyo Clіnic, meningioma cаn cause pressure аnd inflammation inside of the ѕkull and result іn headachөs.
Seizures
Mөningioma οf thө Ьrain maү cause sөizures іn people whο һave neνer beforө had а seizure oг seizure disorder.
Mental Dysfunction
Meningiomas at the base of the sĸull can cause mental dysfunction, such аs cοnfusion and memory loss, that may wοrsen over time as the tumor grows.
Weakness
Weakness of thө muscles in the аrms and legs may be а symрtom of meningioma of tһe spinаl cord, aсcording to thө Mayo Clinic.
CASE REPORT
A 22 year male presented in our emergency with complaints of Headache , Vomiting and Altered sensorium of two days duration. Patient s GCS on Examination was E2V2 M6 and had lower cranial nerve palsies. MRI of brain was done which reveled large extraaxial mass in right parieto-occipital region likely a meningioma measuring approx12-13 cms in size . Due to large size of tumour and deteriorating GCS of the patient he was operated in emergency by Dr Vineet Saggar and after 12 hours of marathon surgery complete tumour removal was achieved . Though patient remained on tracheostomy for few days due to lower cranial palsies which finally recovered and tracheostomy was removed , there was no other neurological deficit. Patient was discharged within 15 days of such a major surgery
Discussion
Surgery is indicated in patients with worsening neurological symptoms and in most patients under 70 who present with a seizure or with any neurological symptoms. If patients are over 70 and present with a seizure or have mild symptoms, they can be followed with scans and undergo surgery if there is evidence of definite growth. However, if there is significant edema or a history of worsening symptoms, age is not a contraindication to surgery. A number of patients are now seen in whom the tumor is found incidently and there is no edema. These patients can be followed with periodic scans, including those with large tumors.Since these tumours are slow growing and exra axial they may attain large sizes if they are located near non eloquent areas as brain continues to compensate due to slow groth rate of tumours . How ever these large sized tumours pose many technical challenges both intra operatively and post operatively.
Apart from increasing surgical and anaesthesia timing large tumours especially near skull base require some degree of brain retraction there by increasing risk of brain edema post operatively. Such tumours some times require extended skull base maneuvers such as extended frontal craniotomies, cranioorbitozygomatic approaches to increase exposure and decrease brain retraction.
M ost of the blood supply of the meningioms is from dura via external carotid system, however venous driange is generally towards venous sinuses and as they grow larger in size they start draining supply of surrounding brain via surrounding piamater .Due to prolonged com pression Autoregulation is also impaired in surrounding brain . So when these tumours are removed it suddeny increased blood supply to surrounding brain there by increasing brain edema or hyper perfusion syndrome.
Our patient had persistent tachycardia inspite of normal hydration and haematocrit following surgery and irritability which settled only few days after the surgery
CONCLUSION
In the end I would like to conclude that meningiomas are slow growing tumours of brain which are amenable to complete surgical removal however sometimes location and size of tumour precludes complete tumour removal,
Very large sized tumours measuring 10-15 cms in size or apprx 1/3 – ¼ volume of brain are rare and pose special challenges to surgeons both intra and post operatively. Such tumours appear like large FOOTBALLS in MR IMAGING require special setup and experienced medical team to counter challenges posed by altered haemodynamics in brain circulation and autoregulation.
Dr. Vineet Saggar (MCh)
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990
http://www.neurosurgeoninchandigarh.com
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
Monday, 12 August 2013
Minimally invasive treatment of vertebral compression fractures at Ivy Hospital by per-cutaneous vertebroplasty by Dr Vineet Saggar (Neuro-Spinal Surgeon)
Minimally
invasive treatment of vertebral compression fractures at Ivy Hospital
by per-cutaneous vertebroplasty by Dr Vineet Saggar
A 54 years old female presented in our OPD with severe pain in back for
past three months. Her X-Ray showed wedge collapse of L1 vertebrae
without canal compromise. She had been on bed rest for three months but
her pain had failed to subside even after full conservative therapy.
She was treated with percutaneous vertebroplasty and her pain was
relieved and she was discharged in fully ambulatory state the next day.
Fig Showing fluoroscopic placement of needle in fractured vertebrae
Fig showing
vertebroplasty cement in fractured vertebrae
Post Operative Ct scan
showing vertebroplasty cement in L1 Vertebrae
Patient just before discharge
Post op pic showing dressing and small incisions
WHAT IS VERTEBROPLASTY AND KYPHOPLASTY?
This
is a technique of injecting bone cement at the site of painful vertebral
compression fractures under fluroscopyand. Painful vertebral osteoporotic
compression fractures lead to significant morbidity and mortality. A painful osteoporotic vertebral fracture can
be a significant burden for patients (and their families), impairing physical
function and quality of life. Independent of pain, there is morbidity
associated with the spinal deformity. In the thoracic spine this is due to
decreased lung capacity (FVC and FEV1). In the lumbar spine compression
fractures also affect lung capacity, probably due to restrictive airway disease
caused by loss of height, and lead to a reduction in abdominal space associated
with loss of appetite and secondary sequel related to poor nutrition. Additionally,
vertebral body compression fractures (VCFs) cause chronic pain, sleep loss,
decreased mobility, depression, and a loss of independence.
The
medications taken for symptomatic relief can lead to further mood or mental
alterations that compound the medical condition. A large prospective study
noted a 23% increase in mortality in women older than 65 years with VCFs
compared with age-matched controls. The mortality rate increases with the
number of vertebrae fractured. Most painful VCFs are treated palliatively, with
bed rest, narcotic analgesics, orthotics, and time. However, bed rest accelerates
bone loss and leads to muscle de conditioning, resulting in increased pain from
both of these mechanisms. The other
treatments for osteoporosis (e.g., hormone replacement, bisphosphonates,
calcitonin) are important for the long term treatment of this disease but often
do not provide short-term pain relief.
INDICATIONS OF VETEBROPLASTY AND
KYPHOPLASTY
PER CUTANEOUS VERTEBROPLASTY has been used in anterior and posterior
stabilization of the spine for metastatic disease, giant cell tumors of,
treatment of vertebral hemangiomas and . vertebral
compression fractures via the transpedicular or paravertebral approach under CT
and/or fluoroscopic guidance has been described.
TECHNIQUE OF VERTEBROPLASTY AND
KYPHOPLASTY
Upon
completing the informed consent process, the patient is placed in the prone
position on the angiography table. Monitoring of blood pressure, heart rate,
and pulse oximetry is done continuously throughout the procedure. Oxygen
supplied via a nasal cannula is used when necessary. Neuroleptic analgesics in
the form of fentanyl (Sublimaze, Abbott Labs, North Chicago,
Ill) and midazolam (Versed, Roche Pharma,
Manati, Puerto Rico) are administered by the
angiography nurse under the direction of the operating physician. The procedure
is performed under strict sterile conditions. All personnel wear surgical masks
and caps in addition to gowns and gloves for the operators, to minimize the
risk of infection. The vertebral body to be treated is localized under
fluoroscopic control and the skin overlying this area is prepped and draped.
Biplane fluoroscopy
is
recommended, as it allows near simultaneous imaging of the stylet tip position
in two planes, thus decreasing the overall procedure time. The anteroposterior
tube is angled in such a way as to maximize the oval appearance of the pedicle
(“looking down the barrel”) (Fig 1). The skin over the center of the pedicle
oval is anesthetized with bupivacaine hydrochloride (0.25%) followed by
deep injection of bupivacaine to and including the periosteum. A small skin
incision is made with a #11 scalpel blade. A disposable 11-gauge Jamshidi
needle is positioned with Fig 1. The pedicle to be punctured is isolated
and marked with the tip of a surgical clamp. The skin, subcutaneous tissues,
and periosteum are anesthetized with 0.25% bupivacaine. Fig 2. After a small
skin incision is made, the Jamshidi needle is advanced nto the pedicle. Notice
that the shaft of the needle (arrow) maintains a bulls-eye appearance in
relation to the pedicular edges (arrowheads) in the anteroposterior plane. Fig
3. In the lateral plane, the shaft of the needle runs parallel to the
superior and inferior cortices of the pedicle (arrows). After the stylet has
been withdrawn, the needle tip is positioned in the middle of the vertebral
body.
Figure 1 Figure 2 Figure 3
its tip in the center of the oval and
advanced until the stylet tip abuts the bone. Lateral fluoroscopy shows the tip
at the level of the upper to midpoint of the pedicle such that advancement of
the needle is within the midportion of theof
the pedicle oval to indicate that the needle is proceeding parallel to
the X-ray beam (Fig 2). The lateral view shows the needle moving roughly
parallel to the superior and inferior edges of the pedicle (Fig 3) or
in a slightly descending course through the pedicle. Minor
adjustments in either plane may be required during needle advancement.
Once the needle tip has traversed the cortex and the pedicle. A slight twisting
motion is used to advance the tip through the cortex, and frequent checking of
needle placement in both planes is required. The anteroposterior view shows the
needle shaft end-on as a circle within the center
pedicle and is located within soft bone marrow, less pressure may be required
to advance the needle into the vertebral body. Care must be taken not to
abrogate the anterior vertebral wall or the endplates. The stylet tip is placed
at or near the junction of the anterior and middle third of the vertebral body
line. Because the stylet tip projects beyond the end of the needle shaft,
removal of the stylet will position the needle end in the middle or
anterior half of the vertebral body (Fig 3). Before injecting the PMMA,
venography is done to exclude needle placement directly within the
basivertebral venous complex and to ensure continuity of the posterior
vertebral wall as evidenced by containment of the contrast material within the
bony trabeculae (Fig 4). We use a hand injection of 5 mL of iohexol (Omnipaque
300, Nycomed,Princeton, NJ) and film in both planes at a rate of two
frames per second. Rapid flow of contrast material into the vena cava and/or
perivertebral veins without visibility of intervening bone marrow indicates
direct communication of the needle tip with a major venous outlet and requires
needle advancement. Once correct placement of the needle is confirmed,
treatment is begun. If a bone biopsy is warranted, a variety of standard,
commercially available biopsy needles can be passed through the Jamshidi shaft
to obtain tissue samples before vertebroplasty One operator injects the
material as the second loads the syringes. The stylet is removed and,
unless blood fills the dead space in a retrograde manner, the dead space is
injected with PMMA using a long 18-gauge spinal needle. The 1-mL syringe is
attached tightly to the shaft port of the Jamshidi needle and injection begins.
The injection pressure required to push the material will increase over time
as the vertebral body fills and the PMMA polymerizes. Injection is performed
under lateral or anteroposterior oblique fluoroscopy ( and particular attention
must be paid to the region of the vena cava and the epidural space as seen on
the venogram. If passage of material into the venous system is when
appropriate.noted, the injection is slowed or halted while the material attains
a thicker consistency. Injection is continued until hemivertebral or
holovertebral filling is achieved, no more material can be pushed into the
body, or extravasation into veins or the disk space is noted. Repositioning of
the needle is not recommended, as the location of the tip will be unknown, and
unwanted vascular embolization may occur. Upon completing the injection,
the needle is removed and hemostasis at the puncture site is achieved by gentle
pressure. The contralateral hemivertebra is then treated in the same fashion.
More than one vertebra can be treated at the same time, depending on the
patient’s tolerance After the procedure, the patient is placed supine and
asked to remain flat for 3 hours to allow complete curing of the PMMA prior to
axial loading. Although patients usually remain overnight, those from our local
area are allowed to return home the same day.
Dr. Vineet Saggar (MCh)
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990
http://www.neurosurgeoninchandigarh.com
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
http://www.slideshare.net/neurosergeonheadhttp://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
Thursday, 18 July 2013
A rare neurovascular surgery at ivy hospital (large p-com aneurysm with fetal pca operated at ivy hospital by dr vineet saggar)
A rare neurovascular surgery at ivy hospital (large p-com aneurysm with fetal pca operated at ivy hospital by dr vineet saggar)
a rare neuro-vascular surgery at ivy
hospital (large p-com aneurysm with fetal pca operated at ivy hospital
by dr vineet saggar)
what
is fetal pca ?
Posterior cerebral arteries are terminal branches of basilar
arteries . Normally in adults it comunicates with anterior circulation or
ICA via small posterior communicating
arteies as shown in figure below
DIAGRAM
OF CIRCLE OF WILLS
The term fetal-type PCA
is also used when there is still a communication with the basilar artery
through a hypoplastic P1 segment of the PCA. Others refer to it only when the
P1 segment is not visible or when the PCA does not fill after contrast
injection of a vertebral artery. In a full FTP(fetal type posterior
circulation), uni- or bilateral, the P1 segment is not visualized on CT or MRI
or does not fill after injection of contrast in a vertebral artery. A partial
FTP, uni- or bilateral, is when the P1 segment is smaller than the PCoA. In an
intermediate posterior circle configuration, the P1 segment is as large as the
PCoA. The adult configuration, finally, is the situation in which the P1
segment is larger than the PCoA, the PCoA sometimes even being absent as shown
in figure below
Kameyama
and Okinaka described four types of what
they called the ‘embryonic PCA’, combining the morphology of the posterior part
and the anterior part of the circle of Willis . In type A, the A1 segment of the
ACA is larger on the side of the FTP than on the contralateral side. In type B,
the A1 is smaller on the side of an FTP. In type C, the ACAs are normal. The
bilateral FTPs were called the ‘primitive-type embryonic derivation’. Although
their definitions are not used in the literature, it could be important to
assess the combination of anterior and posterior part of the circle of Willis,
since it makes a difference if e.g. an ICA has to feed an MCA, both ACAs and a
PCA, compared with an MCA and a PCA only.
Variations
of FTPs a The A1 segment of the ACA is larger on the side of the FTP
than on the contralateral side. b The A1 segments smaller on the side of
an FTP. c ACAs are normal. d ‘Primitive type embryonic
derivation’. e Normal adult type circle of Willis.
CLINICAL AND SURGICAL SIGNIFICANCE
Collateral
circulation in the brain is important for maintaining a sufficient level of cerebral
blood flow in case of obstructive disease in the main afferent arteries. This
arterial network consists of extracranial and intra- cranial routes. The
intracranial collateral vessels comprise the so-called primary collaterals,
consisting of the arterial segments of the circle of Willis, which are used in
case of acute need, and the secondary collaterals such as the ophthalmic artery
and the leptomeningeal vessels, which develop after an ischemic stimulus when
the primary collaterals are insufficient [1] . The leptomeningeal vessels
arepresent or develop between the anterior (ACA), middle (MCA) and posterior
cerebral arteries (PCA). They can represent an important connection between the
internal carotid artery (ICA) and the vertebrobasilar system. Leptomeningeal
collaterals can develop in the majority of circle of Willis configurations.
However, one variant of the circle of Willis, the fetal variant (FTP), makes
leptomeningeal collaterals between the ICA and the vertebrobasilar system
impossible to develop since both the MCA and the PCA are connected to the
internal carotid system and not to the vertebrobasilar system. An important
consequence of the fetal variant of the circle of Willis could be an increased
stroke risk in patients with obstructive arterial disease and following
surgical interventions if accidently PCom is sacrificed or occluded during
surgery for aneurysms. The most rapidly recruited collaterals are the
communicating arteries of the circle of Willis. In FTPs, the ICA covers a
larger area to provide with blood than in the ‘normal’, non-FTP configuration
of the circle of Willis. It is probable that patients with ICA obstruction and
a fullFTP more often encounter ischemic problems than patientswith a ‘normal’
circle, in which the PCoA is preserved and leptomeningeal vessels can develop
between the carotid and the vertebrobasilar system. Patients who also have a
missing contralateral A1 segment, thus having to feed the area of the ACAs, an
MCA and a PCA with 1 ICA could be even more at risk.
CASE
REPORT
A
56 year old female presented in our OPD with history of headache for past one
month . She has had an episode of severe headache followed by loss of
consciousness . CT head plain revealed Sub arachnoid haemorrage in sylvian
fissure and basal cisterns more on left side. CT angiogram revealed multiple
aneurysms: Pcom on left side which was large approx1.5 x 2 cms and small DACA( Distal anterior Cerebral
artery)2 x 3 mm and small Right MCA aneurysm
measuring 4 x 5 mm in size . Also patient had full Fetal type posterior
circulation on left side . Due to location of
SAH and large size of Pcom aneurysm it was identified as site of
rupture. Large size of aneurysm and Fetal posterior circulation made surgery
risky and there was increased risk of ischaemic deficits in posterior
circulation if Fetal Pcom was accidently
clipped during surgery. However Large
Pcom aneurysm was successfully operated
by us and patient was discharged without any deficit.
ANGIGRAPHY
IMAGES SHOWING MULTIPLE ANEURYSMS WITH
LARGE PCOM ANEURYSM
CT ANGIOGRAM SHOWING ABSENT P1 ON LEFT SIDE AND
P2 FILLING VIA LARGE P-COM
PATIENT AT THE TIME OF
DISCHARGE
Dr. Vineet Saggar (MCh)
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990
http://www.neurosurgeoninchandigarh.com
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
http://www.slideshare.net/neurosergeonheadhttp://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
Sunday, 24 March 2013
Tuberculosis still a major Health Problem by Dr. Vineet Saggar (Neurosurgeon in India)
SUNDAY, 24 MARCH 2013
TB STILL A MAJOR HEALTH PROBLEM
Sunday, 24 March 2013 | Nitindra Bandyopadhyay | Chandigarh
Rate : 0/5 Like : 0
Tuberculosis is the second major cause of death due to a single infectious agent after HIV/AIDS. In India it is a major public health problem affecting nearly three million people in 2011 says Dr Vineet Saggar, Spinal Surgeon Ivy Hospital.
According to studies, TB death rate from 1990 to 2009 has dropped from 42 per 1,00,000 to 23 per 1,00,000 respectively. The disease burden is still huge along with its associated socio-economic challenges.
In order to mark the significance of raising awareness about the prevention and management of this pervasive disease, which often turns fatal. World Tuberculosis Day is celebrated globally each year on March 24.
TB, which is caused by the bacteria Mycobacterium tuberculosis, is preventable as well as curable.
Although pulmonary infection, which affects the lungs, is the most common type, the TB bacteria can affect other organs and tissues of the body as well, like the brain, lymph glands, stomach, bones and spine or the backbone.
Spinal tuberculosis is predominantly a disease of the young, the usual age of manifestation being the first three decades of life, thereby affecting people in their most productive years.
The diagnosis of spinal tuberculosis is difficult and it commonly presents at an advanced stage. Spinal tuberculosis progresses gradually and the early manifestations, like back-ache, fever, weakness, weight loss, nausea and vomiting, are often not paid heed to or are mistaken for other health problems, leading to its diagnosis at much advanced stages says the expert.
Though the mainstay of treatment in patients of spinal tuberculosis is Anti Tubercular treatment but surgery is required in cases of neurological deficits due to vertebral collapseor epidural abscess, infact acute vertebral collapse or epidural abscess causing cord compression are surgical emergencies , adds Dr Saggar.
World Tuberculosis Day brings an opportunity to draw attention towards innovations in medical technology made over the period of last 20 years, bringing efficacy and safety in complicated surgical procedures like spine surgeries, making treatment of spine injuries easier and quicker.
Dr. Vineet Saggar (MCh)
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990http://www.neurosurgeoninchandigarh.com
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
http://www.slideshare.net/neurosergeonheadNeuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990http://www.neurosurgeoninchandigarh.com
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
Subscribe to:
Comments (Atom)